Pericardiocentesis
|
Documentation
|
Equipment
Requirements
|
Procedure Note:
Date:
Indication: Diagnostic/therapeutic removal of fluid from the pericardial space
Resident:
Attending:
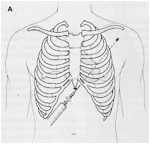
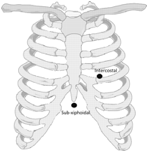
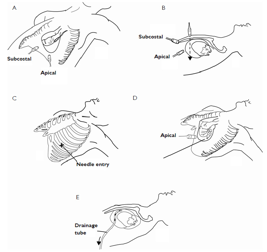
Consent was obtained and a time-out was completed verifying correct patient, procedure, site, and positioning. The patient’s thorax was prepped and draped in sterile fashion. 1% Lidocaine was used to anesthetize the surrounding skin area. Ultrasound was(?)was not used to identify the fluid and observe the needle entering the pericardial space. The needle was introduced into the pericardial space. Appropriate fluid return was obtained and fluid was(?)was not removed for study. The needle was then removed. The patient tolerated the procedure well and there were no complications. Blood loss was minimal.
Chest x-ray was performed to assess for pneumothorax.
Date:
Indication: Diagnostic/therapeutic removal of fluid from the pericardial space
Resident:
Attending:
Consent was obtained and a time-out was completed verifying correct patient, procedure, site, and positioning. The patient’s thorax was prepped and draped in sterile fashion. 1% Lidocaine was used to anesthetize the surrounding skin area. Ultrasound was(?)was not used to identify the fluid and observe the needle entering the pericardial space. The needle was introduced into the pericardial space. Appropriate fluid return was obtained and fluid was(?)was not removed for study. The needle was then removed. The patient tolerated the procedure well and there were no complications. Blood loss was minimal.
Chest x-ray was performed to assess for pneumothorax.